On living low fodmap in a high fodmap world
The health craze had finally caught up to me. In 2011, friends were offering to meet for cold-pressed juice instead of coffee and I often wondered if avocado might hold solutions for my most-pressing problems.
I had been raised in a Long John Silver and Cinnamon Toast Crunch kind of household, so many of the foods that experts were labeling as “super” were ones that I had either never heard of or had tried but dismissed as inedible.
But I was determined to jump on the bandwagon and be the healthiest version of myself. That’s why I decided to start with avocado in the form of a quesadilla. Fast forward to me, a few hours later, on the floor in total pain.
That was my first brush with a food intolerance, and when I hit my thirties, they amped up in a way that demanded I remove my horse blinders.
It wasn’t until I had my daughter that the digestive symptoms became unbearable with bouts of gas sometimes lasting 6-7 hours. Brain fog and fatigue plagued me throughout the day, and insomnia prodded at me at night. Plus, constipation, diarrhea and bloating graduated from once in a while to my everyday state.
Without any real knowledge of what was happening to my body, I tried to fix things by eating “healthier” — overdosing on fermented foods, veggies, and supplements that I had heard were healing.
What I didn’t know then is that healthy eating isn’t a one-size-fits-all formula. What works for one person (likely an influencer on any offending social media site) isn’t guaranteed to work for you. In fact, like Andrea Nakayama1says, it might even wreak havoc on your body.
And that’s certainly what happened to mine. Symptoms worsened until I finally asked for help in the form of a Functional Nutritionist.
With her support, I was able to connect the dots between how I was feeling and what I was putting in my body (nutritionally, mentally and emotionally).
What I discovered was that my body wasn’t a fan of high FODMAP foods.
Here’s how Monash University describes them: “Put simply, FODMAPs are a collection of short-chain carbohydrates (sugars) that aren’t absorbed properly in the gut, which can trigger symptoms in people with IBS. FODMAPs are found naturally in many foods and food additives.”
Food intolerances
This journey is 7 years in the making, and it has been deeply confusing, frustrating, and illuminating.
That’s why I want to share what I’ve learned as well as what has made the biggest impact for healing. This post is not extensive and can definitely NOT be considered medical advice. Again, I’m one person and my body is totally different than yours.
First, a list of my intolerances:
Eggs (not sure if it’s the yolk or the egg white but more than one egg offers Mordor-style type pain)
Sugar snap peas
Almonds (almond milk, almond flour)
Broccoli
Cauliflower
Garlic
Onion
Cherries
Dried goji berries
Coconut (water, milk, and shredded)
Quinoa
Banana
Avocado
Chickpeas
Lentils
Mushrooms (there are some that are lower in fodmaps, but I haven’t tried them yet)
Brussel sprouts
All beans
Cashews
Raisins/cranberries (any dried fruit really)
Bok choy
Tofu
Dates (more than one)
Dairy
Pears
Mangoes
Rye-based breads
Cabbage
I’m sure there are more, but this list extends to what I was used to and what I enjoyed eating.
When I start listing what I can’t eat, I’m often met with, “So what do you eat every day?”
Revolving meals include:
Sesame ginger chicken with white rice and veggies (zucchini, spinach, arugula, carrots, green beans)
Low-fodmap bolognese with gluten free pasta
Baked fish (ahi tuna, cod, salmon, mahi mahi, halibut) with white rice and veggies
Other kinds of baked chicken thighs or legs
Low-fodmap soups of any variety
Oatmeal with add-ons (chia seeds, hemp seeds, blueberries, strawberries, ginger, dates)
Chicken livers, rice, and greens
Rice cakes with peanut butter and salt
Gluten free bagels
Shrimp with gf pasta, garlic olive oil, and red pepper flakes
Low-fodmap cottage pie
I could go on, but the point I’m trying to make is that I still have a lot of options. It took time, but I’ve figured out how to make things taste good without garlic and onion and how to incorporate variety and nutritional density in my diet even though I don’t have access to the entire grocery store.2
Plus, having these food intolerances forced me to get outside of my comfort zone with food and to re-evaluate what I thought I liked. Before dealing with this, I thought I hated arugula. Now I eat it regularly, and I love it.
Speaking of…
Let’s talk about the benefits of my food intolerances
I stopped overeating. I want to say that I loved food, but the truth is that I had an unhealthy obsession with it. Like so many Millennials, I was raised to use food as a Band-Aid when feelings were too big for me. As a result, I used to overeat to the point of discomfort. Or I would eat when I wasn’t hungry. While learning how to heal my gut, I’ve kicked both of those habits (+ the overconsumption of alcohol), and my thoughts around food feel cleaner and less attached than ever before.
I discovered new foods that I love to eat. I won’t lie to you. I often feel a Shakespearean level of yearning for the foods that I can’t eat, but I’ve gained a new appreciation for foods that I was indifferent about before. I mentioned arugula, but I’ve also embraced green onion, cilantro, bean sprouts, and walnuts.
I’ve developed a stronger intuition in the kitchen. I used to put garlic and onion in almost everything. Now that I can’t, I’ve had to get more knowledgeable about and creative with spices and herbs. As a result, I can tell what a dish needs to amp up the flavor even without my comfort ingredients.
Everyone has some level of gut issues. When I tell people about my problems, I often hear that they have issues too. There are foods they can’t tolerate or things that make them feel terrible that they keep eating anyway. Somehow this makes me feel better.
I stopped depending on caffeine. I fell in love with espresso when I first went to Italy, and I carried that newfound love with me well into my twenties and early thirties. Then, I wasn’t able to fall asleep at night anymore, and I needed to eliminate caffeine to see if that was the culprit. (Plus, my nervous system was a mess, so caffeine certainly wasn’t helping.) Now, I still want it, but I don’t need it and that’s a night and day difference from the version of myself I knew ten years ago.
I have a greater appreciation for my body. I used to abuse my body and didn’t realize it — from alcohol to an addiction to productivity. Now I’m able to better measure risk versus reward, and I’m kinder to myself than I’ve ever been. Plus, I’ve learned how to read my body’s rhythms and symptoms with more clarity. I love that I’m turning into my own best health advocate.
Now, the moment that you’ve been waiting for…
How I’m healing my gut
First, I eliminated all of the foods that I thought were the problem. You might recognize this as the Elimination Phase of a gut healing protocol. That alone was life-changing. Sure, mealtimes felt more boring, but I could finally think clearly throughout the day, and I could keep my eyes open past 11am.
Second, my nutritionist advised me to bring in supportive methods like:
Drinking a mix of apple cider vinegar with water at least 15 minutes before eating (starting with 1tsp and then titrating up to 1 tablespoon)3
Taking digestive enzymes after meals4
Taking Calm magnesium powder with aloe vera juice before bed
Eating low doses of fermented foods (titrating up as my body tolerated it)
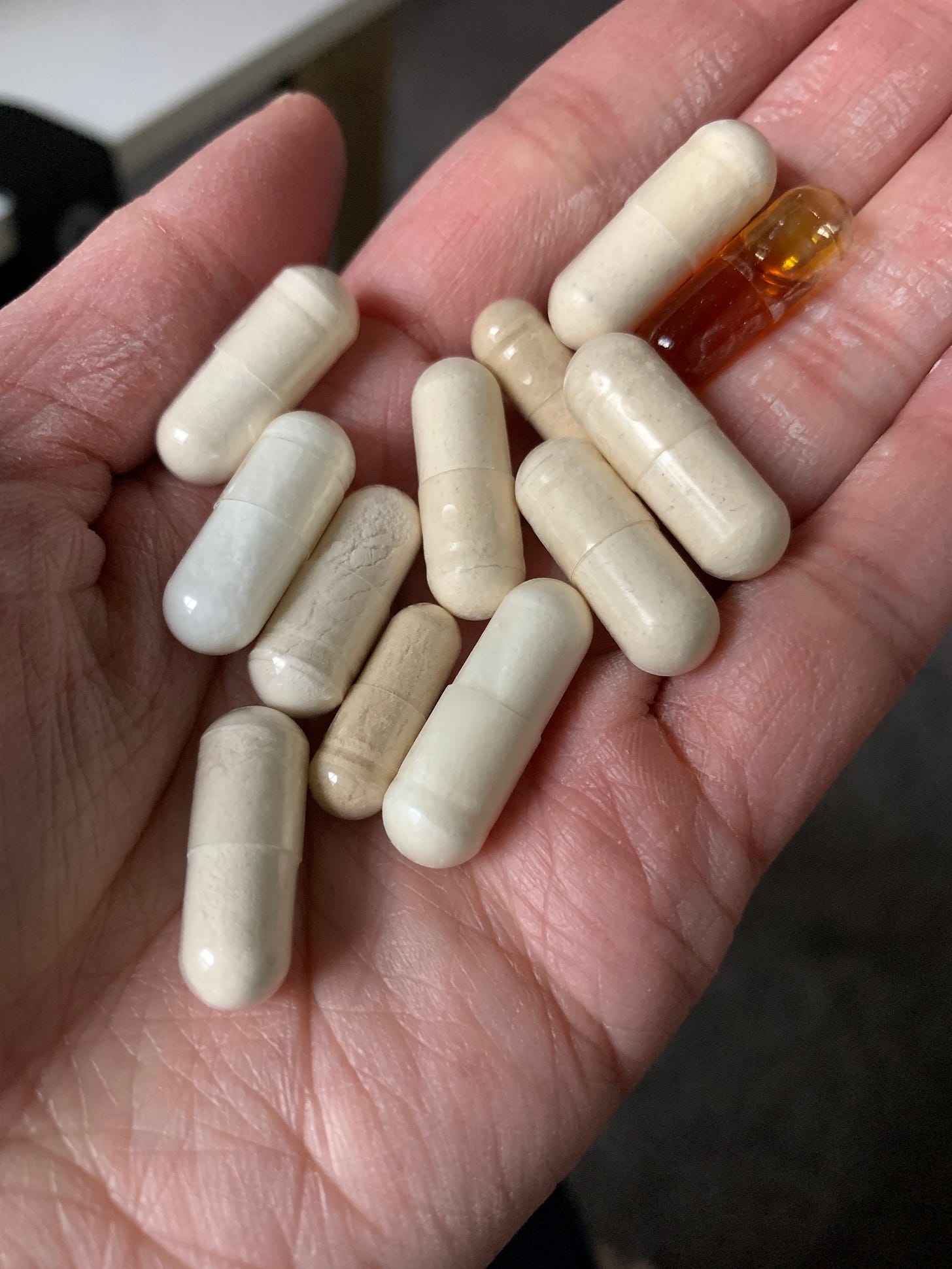
Once we set the foundation, we upped the ante with supplements like:
Probiotics (I had tried a couple of other brands like Seed before but had always had a bad reaction. The trick for me ended up being titration. Starting with a smaller dose and working my way up. Honestly, titration is my preferred course of action when trying to make any change in my life.)
Repairvite (I thought I would hate a powder, but I actually don’t mind it. It might be because I’m now used to taking pills and powders galore.)
Where I’m at now
There is still so much work to be done, but I have been able to reincorporate foods like eggplant and asparagus back into my diet, which is encouraging. Other foods I’ve tried but failed to reincorporate include cauliflower, almond flour, avocado, and mushrooms. Even though I had a reaction from these foods, I’m still counting those food tests as wins because my reactions were less intense compared to previous experiences. Healing happens on a spectrum, after all, and I’ll take my wins where I can get them.
Also, it still sucks to try and eat out or to travel. But, again, not a total loss. It’s challenged me to find other facets of travel to enjoy instead of overindulging in food and alcohol. So, a win, I guess?
Anyway, if we don’t continue to see improvement, we’ll test for parasites, which I imagine will add a whole other set of skills and knowledge to my resume.
In the meantime, I’m going to keep trusting that with the right support, self-kindness, and consistent action, my body will find equilibrium again.
Andrea Nakayama is my go-to source for all things nutrition, my client, and one of the kindest people I have ever met.
I sometimes fantasize about an entire grocery store of low-FODMAP options. I would have choices! It would be dreamy.
There is now a part of my kitchen that may forever smell like ACV. Oh, and for eating out or for travel, I discovered these powder packets. They do contain a sweetener, but I still think it’s worth the convenience and the risk of ACV splashing around uninhibited in my purse.
I have enzymes for foods that don’t irritate my gut and then I have enzymes for fodmap-specific foods, which I use when doing food reintroduction or a taking a risk at a restaurant.